All that you need to know about Prostate Cancer
Not knowing about the ailment one is suffering from can be daunting. Silvertalkies strives to speak to experts to bring you answers to myriad questions that you may have about an ailment. This month we cover Prostate Cancer.
Nidhi Chawla Manoj interviewed Dr. Ali Poonavala, Urologist and Co-Director, Alfa Clinic and Dr. Anoop Amarnath, Director and Consultant, Geriatric Medicine, Apollo Hospitals.
1. What is prostate cancer?
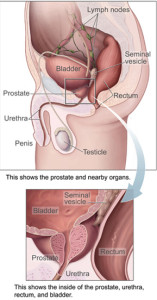
Lets first understand what is Prostate gland. Prostate is a walnut sized solid structure below the urinary bladder, surrounding the urethra, the tube through which urine is discharged outside (Fig. 1). Prostate is made up of microscopic balloons (prostatic acini) which make the prostatic fluid. Structured like a tree, Acini are connected by channels (ducts) which finally empty in the urethra.
(Fig. 1 – Anatomy of the Prostate Gland. Source – Wikipedia)
In the lining of tiny balloons, there is continuous turnover of the cells making the fluid, old ones near surface die, being replaced by new cells from bottom. This well controlled process in some acini gets rebellious, new cells forming faster than required and not forming fluid. This is beginning of prostate cancer.
2. How prevalent is prostate cancer in men? Is any age group more susceptible?
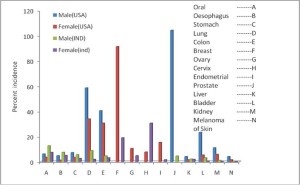
Prostate cancer prevalence is a very interesting topic. There are wide variations between countries and different races within a country. USA reports highest incidence of 272 patients /100,000 in African descendants, falling to 170/100,000 in whites while Tianjin province in China has only 1.9 cases per 100,000 per year! 1 Indian Cancer Registries have recorded incidence of 6-10 per 100,000 and trend seems to be on the rise.2
Regarding age, it is rare before age 50 (< 0.1% of all patients) but peaks between 70-74 years of age. 85% patients are diagnosed after the age of 65 years. 1 However, a word of caution: some may have prostate cancer but will not come to any harm due to it, as it is so called dormant disease.
Fig 3. Variation in various cancers’ incidence between USA and India3
3. What causes prostate cancer? Can it be hereditary? Does lifestyle have a bearing?
We do not know. However, both genetic and life style contribute. Apart from race related variations as mentioned above, there is familial propensity too. For example, risk of having prostate cancer doubles if father or brother had been diagnosed with prostate cancer but quadruples, if both have /had it.
4. What are prostate cancer symptoms and signs?
It is very important to realise that all prostate cancer do not progress. Early curable prostate cancer, unfortunately, produces no symptoms. It is picked up either by screening test or incidentally, when a physician feels the prostate by DRE (Digital Rectal Examination).
Once cancer grows, urinary symptoms like difficulty in passing urine, frequency of urine, blood in urine and even retention (inability to pass urine) may occur. Untreated retention can cause kidney failure too. Rectum may be involved, causing constipation. Symptoms may occur only due to spread of the disease. Pain in the bladder area due to pelvic spread, back ache and even fractures can occur. If a vertebra is affected, even paraplegia can occur.
5. How critical can it be? Is it largely confined to the gland or can it spread?
It is a serious disease and if not detected and treated early, it can spread. Commonest area of spread is to lymph nodes (infection check posts) and axial bones, like spine and pelvic girdle.
6. How is prostate cancer diagnosed?
Prostate cancer is diagnosed by examining prostate tissue under a microscope by a pathologist. This tissue is generally obtained by taking biopsies with a needle or during surgery for retention.
7. Are there any screening tests available to keep a regular tab on it?
The most common screening test is a blood test called serum PSA (Prostate Specific Antigen).
8. What is the recommended norm for these screening tests and how reliable are they?
PSA is a very useful test for follow up of a patient who has been treated for prostate cancer. However, for diagnosis of prostate cancer, it is not reliable. It is increased in any disease affecting the prostate including infections, benign diseases, retention, even DRE.
Recommendations for PSA as a screening test are in a flux due to its inherent limitations as mentioned above and our inability to differentiate between biologically inert and aggressive cancers. However, if a family member is diagnosed to have prostate cancer, PSA testing in male members is recommended early. Advantages and disadvantages of screening must be discussed before embarking on it. There is no blanket approval for indiscriminate use of screening.
9. Can prostate cancer be prevented?
Trials are in progress to see if compounds like Finasteride, Selenium, Vitamin E, Soy, Lycopene and Green tea can be used to prevent cancer prostate.
10. What are different stages of this cancer?
Generally, it starts as a focus in outer part of the gland. In first stage it is entirely confined to the gland. Next, it spreads to seminal vesicles (semen warehouse). Lymph nodes and bone or liver spread are further progression avenues. Serum PSA value, Histological grade, CT or MRI scan as well as bone scan are the tests to define the stage.
11. What are the treatment options available?
Treatment options have to take into account age of the patient, Serum PSA at diagnosis, Histological grading and staging test results.
Early disease, which is organ confined, is curable. In general, the disease runs less aggressive, indolent course in elderly patients (80+) compared to younger (50-65) individuals. Active surveillance, which means observation till it is clear that this is biologically aggressive, is good option for some patients. Other methods to cure include surgery and radiotherapy. Advanced disease cannot be cured and only treated to contain it. Initially Hormone therapy and later, chemotherapy are used for limiting advanced disease.
12. Could you please elaborate on benefits and risks of each treatment?
Surgery: Benefit is the immediate removal of cancer with lymph nodes (check posts) which helps in final staging. Risks include those of a major operation, i.e. bleeding, infection, lung and heart complications etc. Peculiar and distressing problem include losing control over urination (incontinence) and impotence. Generally, these are temporary but for about 10%, may be lifelong.
Radiotherapy: Obvious advantage is avoiding a major surgery with risks as mentioned. However, there is no confirmation of cure and no final staging since no tissue is available. Apart from early irritating urinary frequency and diarrhoea which improves, incontinence and impotence sometimes is seen later on. There is also small risk of developing other type of cancer due to radiotherapy itself.
13. Is surgical removal of the gland beneficial?
In younger patients with aggressive disease, surgery offers better cure rates than radiotherapy does.
14. Are there any alternate forms of treatment available?
Cryotherapy (using liquid Argon gas to freeze tissue), RF (Radio Frequency) ablation, and HIFU (High Intensity Focussed Ultrasound) are being used in some selected cases.
15. How long is the recovery period?
Since patient may have different forms of treatment depending on the extent and age, it is difficult to give approximate time frame here. Surgery, especially keyhole type, is associated with excellent recovery in experienced hands. Within 2-3 weeks of catheter removal, urinary control becomes acceptable in upto 95% patients.
16. Are there any chances of relapse and in what form?
Relapse is rare in early stages and common as the disease stage is higher on initial presentation. If surgery was the initial therapy, distant relapse (metastasis) is seen, generally in bones of spine or in lungs or liver. After radiotherapy, both, local and distance failure occurs.
17. Once treated does one requires regular check-ups to look out for relapse?
Absolutely necessary to have a good follow up with the treating team of Physician, Urologist and Oncologist. Depending on the progress, initially 3 monthly and later 6-12 monthly assessments are done to detect relapses early. Further treatment can be given while disease volume is low and patient is fitter.
If Hormone treatment has to be given, there can be significant loss of bone and that can lead to fracture of hip or spine. So these patients need regular Blood Calcium and Bone Density tests and treatment and exercises to prevent bone loss.
18. How does prostate cancer affect a patient?
Though so intimately associated with the urinary system, Prostate is a sexual organ and has no role, except being a nuisance, for the urinary tract!
Prostatic fluid is part of semen. This fluid has substances (proteases) which liquefy coagulated semen and help to sustain the sperm’s journey, from vagina, through the uterus, towards the ovum. Prostate gland function is regulated by the male hormone testosterone.
Since the disease affects a very critical area of bodily function and involves sexual health too, self-image of the patient may take a beating especially if he suffers from complications like impotence or incontinence. One may need to wear diapers on a day to day basis and may find simple activities, like morning walks restrictive as it makes leak worse.
Prostate cancer being a disease of elderly, there are medical financial and social issues which may have considerable impact on the choice of treatment apart from the disease related factors.
19. Any advice for patients of prostate cancer?
They must make friends with this enemy within. Seek expert advice as well as help from support groups. Define priorities. Do your home-work. Do not hesitate to question treatment plans.
Above all, be optimist. Be positive. Remember, most (75%) prostate cancer patients live long enough with their cancer.
Acknowledgement:
1.Campbell and Walsh Text book of Urology 9th Edition 2008 Ed in Chief Alan Wein vol.3 chapters 90-105.2854-3117
2.Trends in the Prostate Cancer Incidence in India. Balkrishna B YeoleAsian Pacific J Cancer Prev, 9, 141-144
3.Cancer Scenario in India with Future Perspectives Imran Ali*, Waseem A. Wani and Kishwar Saleem Cancer Therapy Vol 8, 56-70, 2011.
 About the expert: Dr. Ali Poonawala is co-Director of Alfa Clinic, (www.alfaclinic.net ) Fertility, Maternity and Urology Centre in Bangalore and is a visiting consultant since 1993 and Head of Department of Urology at St. Martha’s Hospital since 1995. Being a General Urologist, Prostate and Kidney Stones are his primary work areas; Laparoscopic Urological work and Male Infertility are closer to his heart. He is also President elect of Karnataka Urologists Association (KUA) for 2014-15. He loves cycling and uses it for daily commuting to work, come rain or shine!
About the expert: Dr. Ali Poonawala is co-Director of Alfa Clinic, (www.alfaclinic.net ) Fertility, Maternity and Urology Centre in Bangalore and is a visiting consultant since 1993 and Head of Department of Urology at St. Martha’s Hospital since 1995. Being a General Urologist, Prostate and Kidney Stones are his primary work areas; Laparoscopic Urological work and Male Infertility are closer to his heart. He is also President elect of Karnataka Urologists Association (KUA) for 2014-15. He loves cycling and uses it for daily commuting to work, come rain or shine!
 About the expert: Dr. Anoop Amarnath is Director and Consultant, Geriatric Medicine, Apollo Hospitals, Bangalore. He has a specialisation in Geriatric Medicine from the Royal College London with certification in Geriatric Nephrology from the American Society of Nephrology and has been practicing since 2004.
About the expert: Dr. Anoop Amarnath is Director and Consultant, Geriatric Medicine, Apollo Hospitals, Bangalore. He has a specialisation in Geriatric Medicine from the Royal College London with certification in Geriatric Nephrology from the American Society of Nephrology and has been practicing since 2004.
Comments
You may like to read:

Health and wellness
Five Lifestyle Changes To Ease Bladder Control

jessica smith
5 mins read

Health and wellness
Five things to keep in mind when considering organ donation

sunayana singh, ceo of organ india, an initiative of the parashar foundation
3 mins read

Health and wellness
How NURA Uses AI-Enabled Screening to make a difference in Preventive Healthcare

Silver Talkies
4 mins read

Post a comment